Biologics like dupilumab are a newer type of eczema treatment that target an overreactive response in the body’s immune system that leads to inflammation and eczema symptoms. Along with a proactive skincare regimen, biologics may provide people with treatment-resistant, moderate-to-severe eczema an avenue to symptom relief. Since biologics for eczema have only been FDA-approved since 2017, scientists are still learning about their long-term safety and efficacy.
Here’s what you need to know about biologics for eczema, including how they work, which treatments are FDA approved, what side effects may occur, and who makes a good candidate for biologic treatment.
What are biologics?
Biologics are prescription-only medical therapies that get their name from being derived from living organisms as opposed to being made completely from chemicals that are synthesized in a lab.
Sometimes called “large molecule” drugs, biologics provide a specific therapy for a specific issue instead of more general treatment. The targeted nature of biologics within the immune system means that they are not considered to be immunosuppressants.
At the same time — and perhaps confusingly — biologics are known as “systemic treatments” because they travel throughout the bloodstream and affect cells throughout the body.
Finally, because they are created from living organisms, biologics are also typically more difficult — and thus more expensive — to produce.
How do biologics for eczema work?
Scientific studies have shown that people with eczema likely have an overreactive, elevated immune system response that causes inflammation and decreased skin barrier function. Biologics try to target the immune system's response that causes these issues.
To break this process down, we need to start with antibodies. Antibodies are proteins that the immune system creates to defend against or destroy viruses, bacteria, and other disease-causing microbes. They are an important part of your immune system’s response to threats.
Biologics for eczema involve the creation of lab-modified antibodies called monoclonal antibodies, or mAbs (which is why many biologic drug names end in -mab). Instead of targeting microbes, mAbs target the immune cell (or T cell) responses that lead to inflammation and decrease skin barrier function.
In particular, the mAbs target immune system chemical “messengers” called cytokines — specifically a type of cytokines called interleukins (ILs) — that are “sent” by the T cells in order to “tell” other types of immune cells that they need to react to a threat.
If the ILs are not intercepted, these “alerted” immune cells will trigger an unnecessarily elevated immune response. To stop this unnecessary response from occurring, the monoclonal antibodies block the “signal receiver” —- the receptor — on the immune system cells where the interleukin would “dock.”
The metaphor often used here is that of a key and lock. The immune system cell is the lock. The IL is the key. If the IL key enters the lock, the immune system's response is triggered. The monoclonal antibodies are specifically designed to also fit within the keyhole so that the IL can’t enter the lock and the immune system response can’t be triggered.
There are many types of ILs thought to be involved in the immune system’s response to eczema triggers, and different biologic medications target different ILs.
How do you take biologics for eczema?
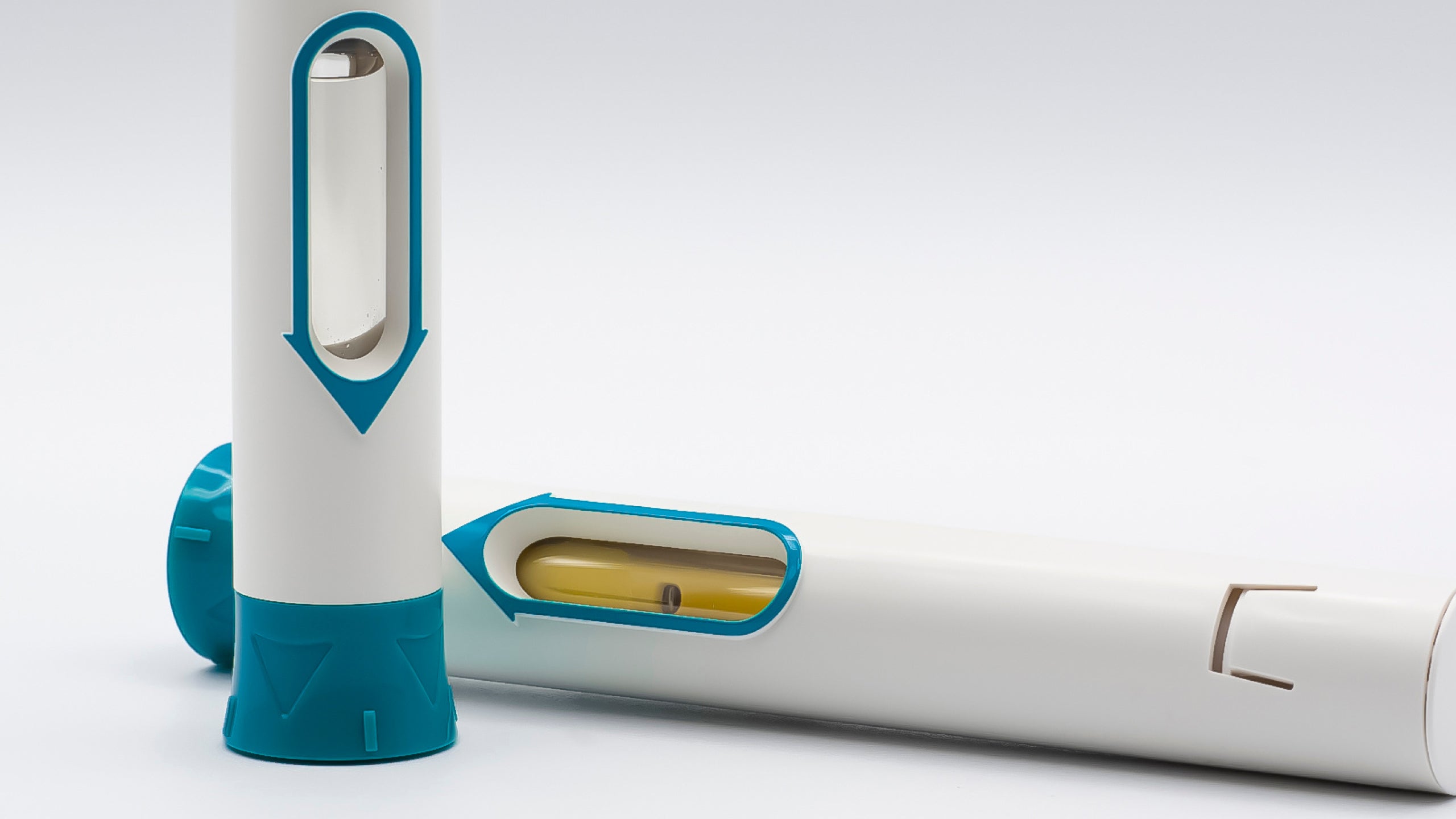
The biologics used in eczema therapy are delivered subcutaneously via injectables, aka a shot. They are not available as a pill because they’re sensitive to changes in light and temperature and can’t pass through the digestive system without disruptions to their structure.
What's the difference between JAK inhibitors and biologics for eczema?
Janus kinase (JAK) inhibitors are “small molecule drugs” (read: synthetic drugs) that inhibit “messages” being sent via an entire cytokine “communication pathway” (the JAK-STAT pathway) instead of targeting the reception of a specific cytokine or IL. Since they are synthetic, they can be taken orally, via capsule. They are available via prescription only.
For more information, please see our article on JAK inhibitors for eczema.
What are the FDA-approved biologics for atopic dermatitis?
According to the National Eczema Association, there are “over 25 different biologic drugs with more than 10 unique IL and cytokine targets” currently in development as of March 2022. But there are currently only 2 biologic eczema treatments approved by the FDA.
Dupixent (Dupilumab)
Dupixent was approved as a prescription treatment for moderate-to-severe atopic dermatitis by the FDA:
- In 2017 for adults
- In 2019 for teens (aged 12-17 years)
- In 2020 for children (aged 6-11 years)
- In 2022 for young children (aged 6 months-5 years)
It targets 2 interleukins, IL-4 and IL-13. It can be given to you by a doctor or self-administered and comes either as a pre-filled syringe or pen. The dosage amount and frequency of injection are dependent on your age and weight.
Adbry (Tralokinumab-Idrm)
Adbry (tralokinumab-ldrm) was approved as a prescription treatment for moderate-to-severe atopic dermatitis in adults 18+ by the FDA in 2021.
It targets 1 interleukin, IL-13. It can be given to you by a doctor or self-administered and comes in a pre-filled syringe. The dosage amount and frequency of injection are dependent on your age and weight.
Do biologics have side effects?
Biologics do come with side effects. The most common side effects include eye irritation and inflammation, injection site reaction, cold sores, higher-than normal white blood cell count (eosinophilia), and joint pain.
It is possible to be allergic to biologics. Serious but rarer side effects that require immediate medical attention include vision changes, hives, difficulty breathing, swelling of the face/lips/tongue/throat, dizziness, fainting, and lightheadedness.
How long do you take biologics for?
Since biologics for eczema were first FDA approved in 2017, their long-term efficacy is unknown. Doctors recommend that once you start using a biologic for eczema, you stay on it continuously—-if you start and stop, it is possible to develop antibodies that make the drug less effective over time.
Who is a good candidate for biologics for eczema?
Biologics are typically reserved for people with treatment-resistant, moderate-to-severe eczema. Since topical treatments are easier (and likely cheaper, depending on your insurance) to obtain and use, your doctor will generally start by prescribing those first and will only consider biologics if topical treatments aren’t providing sufficient relief.
Are biologics safe for kids?
Biologic treatments for eczema are relatively new, and the scientific community will be learning about their safety and efficacy for decades to come. However, Dupixent has been approved by the FDA for children ages 6 months+. Your doctor will likely try other forms of eczema treatment before recommending a biologic.
For parents of children with eczema, we recommend our guide to baby eczema and our guide to toddler eczema.
Questions to ask your dermatologist about biologics
Planning a trip to the dermatologist to explore whether biologics are an option for you? Here are a few questions that can help guide that discussion.
- Knowing my health history and risk factors, am I a good candidate for biologics?
- When should I start treatment, and is there anything I should do to prepare?
- What side effects should I watch out for? And what should I do if I experience side effects?
- How long should I wait before contacting you if I don’t experience results?
- Based on your knowledge of my skin health, what kind of results can I expect?
- If the biologic provides relief, do you anticipate recommending long-term use?
- What skincare regimen should I practice while taking biologics?
See our article on questions to ask your dermatologist about eczema for ways to make your appointment be as informative and go as smoothly as possible.
Biologics and Skincare
If you’re struggling with moderate-to-severe eczema and have tried other treatments with no results, speak with your dermatologist to see if you are a good candidate for biologics.
Meanwhile, keep in mind that biologics are often taken as part of a multi-pronged approach to managing eczema symptoms. Patients who take biologics will likely still need skincare that relieves dryness associated with eczema-prone skin. Gladskin’s Eczema Cream with Micreobalance® restores bacterial balance to the skin microbiome while moisturizing and is clinically proven to reduce eczema symptoms.
Explore the science behind Gladskin and shop our steroid-free, microbiome friendly products today.